Natural anti–malarials: A bright hope
Keywords:
Malaria, Plasmodium, drug resistance, combination therapy, natural anti–malarialsAbstract
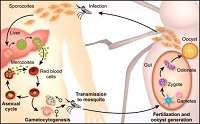
Malaria is still an ever–continuing epidemic that claims a large number of lives in tropical and subtropical regions of the globe. The alarming rate at which the parasite, Plasmodium has developed resistance to currently used anti–malarial drugs makes it imperative to search for newer and more effective therapeutic agents. In this context, during last few decades several fundamental researches have been conducted to explore novel anti–malarial formulations. However, recent scientific evidences have indeed demonstrated that a variety of plant compounds may check the survival of Plasmodium both in vitro and in vivo. But, there is a need to evaluate and advocate their efficiency in a proper way, because reliable data on the clinical pharmacology and safety of such formulae are extremely scarce, preventing a responsible consideration of their potential benefits. Conclusively, after reviewing literatures it is very clear that plants with anti–malarial activity do not have fully defined this therapeutic property. Therefore, it is necessary to encourage multidisciplinary and interdisciplinary research, mostly those related to natural products enabling the discovery of new and appropriate anti–malarial pharmaceuticals.
References
. Snow RW, Guerra CA, Noor AM, Myint HY, Hay SI. The global distribution of clinical
episodes of Plasmodium falciparum malaria. Nature 2005; 434: 214–117.
. World Health Organization. The World Health Report. Health Systems Financing: the Path to Universal Coverage. World Health Organization, Geneva. 2010; pp 96.
.Pasvol G. Protective hemoglobinopathies and Plasmodium falciparum transmission. Nature Genetics, 2010; 42, 284-285. doi:10.1038/ng0410-284.
. Prudencio M, Mota MM, Mendes AM. A toolbox to study liver stage malaria. Trends Parasitol. 2011; 27: 565–574.
. Sahu NK, Sahu S, Kohli DV. Novel molecular target for anti–malarial drug development. Chem. Bio. Drug Design 2008; 71: 287–297.
. Pink R, Hudson A, Mouries MA, Bendig M. Opportunities and challenges in antiparasitic drug discovery. Nature Rev. Drug Discovery 2005; 4: 727–740.
. Wiwanitkit V. Plasmodium and host lactate dehydrogenase molecular function and biological pathways: implication for anti–malarial drug discovery. Chem. Bio. Drug Design 2007; 69: 280–283.
. Udeinya IJ, Brown N, Shu EN. Fractions of an anti–malarial neem–leaf extract have activities superior to chloroquine, and are gametocytocidal. Ann. Trop. Med. Parasitol. 2006; 100(1): 17–22.
. Guadalupe E, Garcia L, Rodriguez JB. Current status and progress made in malaria chemotherapy. Curr. Med. Chem. 2007; 14: 289–314.
. Ridley RG. Medical need, scientific opportunity and the drive for antimalarial drugs Nature 2002; 415(6872): 686–693.
. Ibezim EC, Odo U. Current trends in malaria chemotherapy. Afr. J. Biotechnol. 2008; 7: 349–356.
. Guerra F. The introduction of cinchona in the treatment of malaria. J. Trop. Med. Hyg. 1977; 80: 135–140.
. Achan J, Talisuna AO, Erhart A, Yeka A, Tibenderana JK, Baliraine FN, Rosenthal PJ, D'Alessandro U. Quinine, an old anti–malarial drug in a modern world: role in the treatment of malaria. Malar. J. 2011; 10: 144–156.
. Coatney GR. Pitfalls in a discovery: the chronicle of chloroquine. Am. J. Trop. Med. Hyg. 1963; 12: 121–128.
. Kurcer MA, Simsek Z, Zeyrek FY, Atay S, Celik H, Kat I, Topluoglu S. Efficacy of chloroquine in the treatment of Plasmodium vivax malaria in Turkey. Ann. Trop. Med. Parasitol. 2004; 98: 447–451.
. Baird JK, Wiady I, Fryauff DJ, Sutanihardja MA, Leksana B, Widjaya H, Kysdarmanto, Subianto B. In vivo resistance to chloroquine by Plasmodium vivax and Plasmodium falciparum at Nabire, Irian Jaya, Indonesia. Am. J. Trop. Med. Hyg. 1997; 56: 627–631.
. Phillips-Howard PA, Steffen R, Kerr L, Vanhauwere B, Schildknecht J, Fuchs E, Edwards R. Safety of mefloquine and other anti–malarial agents in the first trimester of pregnancy. J. Travel Med. 1998; 5(3): 121–126.
. Sweeney TR. The present status of malaria chemotherapy: mefloquine, a novel anti–malarial. Med. Res. Rev. 1981; 1: 281–301.
. Price RN, Uhlemann AC, Brockman A, McGready R, Ashley E, Phaipun L, Patel R, Laing K, Looareesuwan S, White NJ, Nosten F, Krishna S.. Mefloquine resistance in Plasmodium falciparum and increased pfmdr1 gene copy number. Lancet 2004; 364(9432): 438–47.
. Yavo W, Bla KB, Djaman AJ, Assi SB, Basco LK, Mazabraud A, Koné M.In vitro susceptibility of Plasmodium falciparum to monodesethylamodiaquine, quinine, mefloquine and halofantrine in Abidjan (Côte d.Ivoire) Afr. Health Sci. 2010; 10(2): 111– 116.
. Basco LK, Le Bras J. In vitro activity of halofantrine and its relationship to other standard anti–malarial drugs against African isolates and clones of Plasmodium falciparum. Am. J. Trop. Med. Hyg. 1992; 47(4): 521–527.
. Frosch T, Popp J. Structural analysis of the anti–malarial drug halofantrine by means of Raman spectroscopy and density functional theory calculations. J. Biomed. Opt. 2010; 15(4): 041516. doi: 10.1117/1.3432656.
. Salako LA, Sowunmi A, Walker O. Evaluation of the clinical efficacy and safety of halofantrine in falciparum malaria in Ibadan, Nigeria. Trans. R. Soc. Trop. Med. Hyg. 1990; 84(5): 644–647.
. Putrianti ED, Silvie O, Kordes M, Borrmann S, Matuschewski K. Vaccine–like immunity against malaria by repeated causal–prophylactic treatment of liver–stage Plasmodium parasites. J. Infect. Dis. 2009; 199(6): 899–903.
. Fernando D, Rodrigo C, Rajapakse S. Primaquine in vivax malaria: an update and review on management issues. Malar. J. 2011; 10: 351 http://www.malariajournal.com/content/10/1/351.
. Dominguez JN, Leon C, Rodrigues J, Gamboa de Domínguez N, Gut J, Rosenthal PJ. Synthesis and anti–malarial activity of sulfonamide chalcone derivatives. Farmaco. 2005; 60(4): 307–311.
. Triglia T, Menting JGT, Wilson C, Cowman AF. Mutations in dihydropteroate synthase are responsible for sulfone and sulfonamide resistance in Plasmodium falciparum. Proc Natl. Acad. Sci. USA. 1997; 94: 13944–13949.
. Michel R. Comparative study of the association of sulfalene and pyrimethamine and of sulfalene alone in mass chemoprophylaxis of malaria. Med. Trop. 1968; 28: 488–494.
. Nzila A. The past, present and future of antifolates in the treatment of Plasmodium falciparum infection. J. Antimicrob. Chemother. 2006; 57: 1043–1054.
. White NJ. Preventing anti–malarial drug resistance through combinations. Drug Resist. Update 1998; 1: 3–9.
. Willcox M. Artemisia species: From traditional medicines to modern anti–malarials–and back again. J. Altern. Compliment Med. 2009; 15: 101–109.
. Deprez–Poulain R, Melnyk P. 1,4–Bis(3–aminopropyl) piperazine libraries: from the discovery of classical chloroquine–like anti–malarials to the identification of new targets. Comb. Chem. High. Throughput Screen 2005; 8: 39–48.
. Jones MK, Good MF. Malaria parasites up close. Nat. Med. 2006; 12: 170–171.
. Winter RW, Kelly JX, Smilkstein MJ, Dodean R, Bagby GC, Rathbun RK, Levin JI, Hinrichs D, Riscoe MK. Evaluation and lead optimization of anti–malarial acridones. Exp. Parasitol. 2006; 114: 47–56.
. Upadhyay RK, Ahmad S. Ethno–medicinal plants and their pharmaceutical potential. J. Pharm. Res. 2012; 5(4): 2162–2173.
. Ziegler HL, Staerk D, Christensen J, Hviid L, Hagerstrand H, Jaroszewski JW. In vitro Plasmodium falciparum drug sensitivity assay: inhibition of parasite growth by incorporation of stomatocytogenic amphiphiles into the erythrocyte membrane. Antimicrob. Agents Chemother. 2002; 46: 1441–1446.
. Kalauni SK, Awale S, Tezuka Y, Banskota AH, Linn TZ, Asih PB, Syafruddin D, Kadota S. Anti–malarial activity of cassane– and norcassane–type diterpenes from Caesalpinia crista and their structure–activity relationship. Biol. Pharm. Bull. 2006; 29: 1050–1052.
. Portet B, Fabre N, Roumy V, Gornitzka H, Bourdy G, Chevalley S, Sauvain M, Valentin A, Moulis C. Activity–guided isolation of antiplasmodial dihydrochalcones and flavanones from Piper hostmannianum var. berbicense. Phytochemistry 2007; 68: 1312–1320.
. Roth GN, Chandra A, Nair MG. Novel bioactivities of Curcuma longa constituents. J. Nat. Prod. 1998; 61: 542–545.
. Deharo E, Bourdy G, Quenevo C, Munoz V, Ruiz G, Sauvain M. A search for natural bioactive compounds in Bolivia through a multidisciplinary approach. Part V. Evaluation of the anti–malarial activity of plants used by the Tacana Indians. J. Ethnopharmacol. 2001; 77: 91–98.
. Marcela E, Silvia B, Jaime C, Pilar P. Effect of Solanun nudum extracts on the liver of mice infected with Plasmodium berghei. Amer. J. Chinese Med. 2001; 29: 477–484.
. Oliveira FQ, Andrade–Neto V, Krettli AU, Brandao MGL. New evidences of anti malarial activity of Bidens pilosa root correlated with polyacetylene and flavonoids. J. Ethnopharmacol. 2004; 93: 39–42.
. Andrade-Neto VF, Brandão MGL, Stehmann JR, Oliveira LA, Krettli AU. Anti–malarial activity of Cinchona like plants used to treat fever and malaria in Brazil. J. Ethnopharmacol. 2003; 87: 253–56.
. Okunade AL, Lewis WH. Oleanene constituents of Lantana cujabensis. Fitoterapia 2004; 75: 327–331.
. McPhail KL, Correa J, Linington RG, Gonzalez J, Ortega-Barría E, Capson TL, Gerwick WH.Anti–malarial linear lipopeptides from a Panamanian strain of the marine Cyanobacterium Lyngbya majuscula. J. Nat. Prod. 2007; 70: 984–88.
. Bhat GP, Surolia N. In vitro anti–malarial activity of extracts of three plants used in the traditional medicine of India. Am J Trop Med Hyg 2001; 65(4): 304–308.
. Saxena S, Pant N, Bhakuni RS. Anti–malarial agents from plant sources. Cur. Sci. 2003; 85: 1314–1326.
. Gupta SK, Prakash J, Srivastava SV. Validation of claim of Tulsi, Ocimum sanctum Linn. as a medicinal plant. Indian J. Exp. Biol. 2002; 40(7): 765–73.
. Rahman NNNA, Furuta T, Kojima S, Tabane K, Ali-Mohd M. In vitro and in vivo study revealed that malarias medicinal plants, Piper sarmentosum, Andrographis paniculata and Tinospora crispa produce considerable anti–malarial effect. J. Ethnopharmacol. 1999; 64: 249–254.
. Coppi A, Cabinian M, Mirelman D, Sinnis P. Anti–malarial activity of Allicin, a biologically active compound from garlic gloves. Antimicrob. Agents Chemothe. 2006; 50(5): 1731–1737.
. Rucker G, Walter RD, Manns D, Mayer R. Antimalarial activity of some natural peroxides. Planta Med. 1991; 57: 295–296.
. Bray DH, Warhurst DC, Connolly JD, O’Neill MJ, Phillipson JD. Plants as source of antimalarial drug. Pt.7 activity of some species of Meliaceae plants and their constituent limoids. Phytother. Res. 1990; 4: 29–35.
. Joshi SP, Rojatkar SR, Nagasampagi BA. Antimalarial activity of neem (Azadirachta indica). J. Med. Aromat. Plant Scie. 1998; 20: 1000–002.
. Weenen H, Nkunya M H H, Bray DH, Mwasumbi L B, Kinabo LS, Kilimali VAEB Wijnberg JBPA. Antimalarial compounds containing an a, b-unsaturated carbonyl moiety from Tanzanian medicinal plants. Planta Med 1990; 56: 371–73.
. Kardono LBS, Angerhofer CK, Tsauri S, Padmawinata K, Pezzuto JM, Kinghorn AD. Cytotoxic and antimalarial constituents of the roots of Eurycoma longifolia. J. Nat. Prod. 1991; 54: 1360–1367.
. Koumaglo K, Gbeassor M, Nikabu O, De Souza C, Werner W. Effects of three compounds extracted from Morinda lucida on Plasmodium falciparum. Planta Med. 1992; 58: 533–534.
. Jenett-Siems K, Siems K, Jakupovic J, Solis PN, Gupta MP, Mockenhaupt FP, Bienzle U, Eich E.Sipandinolide: a butenolide including a novel type of carbon skeleton from Siparuna andina. Planta Med. 2000; 66(4): 384-385.
. Figueiredo, JN, Raz B, Sequin U. Novel quinone methides from Salacia kraussii with in vitro antimalarial activity. J. Nat. Prod. 1998; 61: 718–723.
. Bringmann G, Günther C, Saeb W, Mies J, Wickramasinghe A, Mudogo V, Brun R. Ancistrolikokines A–C: New 5,8¢-coupled naphthylisoquinoline alkaloids from Ancistrocladus likoko. J. Nat. Prod. 2000; 63: 1333–1337.
. Joshi SP, Rojatkar SR, Nagasampagi BA. Antimalarial activity of Xanthium strumarium. J. Med. Aromat. Plant Scie. 1997; 19: 366–68.
. Mishra K, Dash AP, Swain BP, Dey N. Anti-malarial activities of Andrographis paniculata and Hedyotis corymbosa extracts and their combination with curcumin. Malar. J. 2009; 8: 26-35.
. Reddy RC, Vatsala PG, Keshamouni VG, Padmanaban G, Rangarajan PN. Curcumin for malaria therapy. Biochem. Biophys. Res. Commun. 2005; 326: 472–474.
. Nandakumar DN, Nagaraj VA, Vathsala PG, Rangarajan P, Padmanaban G. Curcumin–artemisinin combination therapy for malaria. Antimicrob. Agents Chemother. 2006; 50: 1859–1860.
. Mishra K, Dash AP, Dey N. Andrographolide: A novel anti–malarial diterpene lactone compound from Andrographis paniculata and its interaction with Curcumin and Artesunate. J. Trop. Med. 2011; 11: Article ID 579518.